Sexually Transmitted Infections (STIs) represent a complex group of infections with various modes of transmission and significant implications for public health. This exploration delves into the intricacies of STI transmission, the importance of prevention strategies, and the role of education in fostering responsible sexual health practices.
1. Modes of STI Transmission:
1.1 Sexual Transmission: The primary mode of STI transmission is through sexual contact, encompassing vaginal, anal, and oral sex. Unprotected intercourse with an infected partner significantly increases the risk of acquiring STIs, including bacterial, viral, and parasitic infections.
1.2 Vertical Transmission: Some STIs can be transmitted from an infected mother to her baby during childbirth or through breastfeeding. Vertical transmission is particularly relevant for infections like HIV, syphilis, and herpes simplex virus (HSV).
1.3 Blood-to-Blood Transmission: Certain STIs, such as HIV and hepatitis B, can be transmitted through exposure to infected blood. This can occur through sharing needles among intravenous drug users or through contaminated blood products.
2. Common STIs and their Transmission:
2.1 Chlamydia and Gonorrhea: These bacterial infections are primarily transmitted through unprotected sexual intercourse, affecting the genital tract, rectum, and throat. They may also be transmitted from an infected mother to her baby during childbirth.
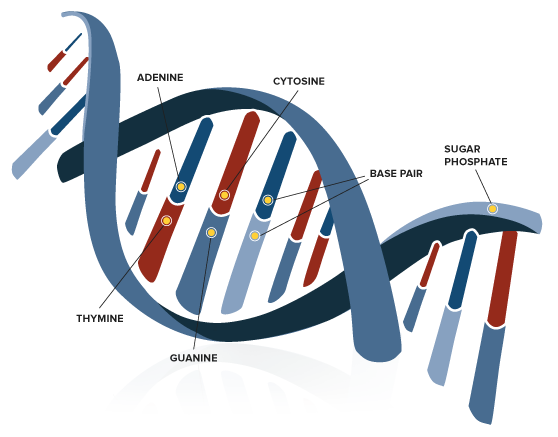
2.2 HPV (Human Papillomavirus): HPV is a viral infection transmitted through skin-to-skin contact. It commonly spreads through sexual contact, including vaginal, anal, and oral sex. Certain high-risk HPV types can lead to cervical cancer.
2.3 HIV (Human Immunodeficiency Virus): HIV is primarily transmitted through unprotected sexual intercourse, the sharing of contaminated needles among intravenous drug users, and from mother to child during childbirth or breastfeeding. It can also be transmitted through blood-to-blood contact.
2.4 Herpes Simplex Virus (HSV): HSV is transmitted through direct contact with the sores or fluids of an infected person. It can be spread through vaginal, anal, or oral sex, as well as through kissing. Vertical transmission can occur from an infected mother to her baby.
2.5 Syphilis: Syphilis is a bacterial infection transmitted through direct contact with a syphilis sore, often during vaginal, anal, or oral sex. It can also be transmitted from an infected mother to her baby during childbirth.
3. Prevention Strategies:
3.1 Safe Sex Practices: Consistent and correct use of barrier methods, such as condoms, during sexual intercourse is a highly effective strategy for preventing the sexual transmission of STIs. Condoms act as a physical barrier, reducing the risk of contact with infectious fluids.
3.2 Vaccination: Vaccination is a preventive measure against certain STIs. The HPV vaccine, for example, protects against several high-risk HPV types, reducing the risk of cervical cancer. The hepatitis B vaccine is effective in preventing hepatitis B infection.
3.3 Regular STI Testing: Routine STI testing is crucial, especially for individuals with multiple sexual partners or engaging in high-risk behaviors. Early detection allows for prompt treatment and prevents the spread of infections to others.
3.4 Pre-Exposure Prophylaxis (PrEP): PrEP involves taking antiretroviral medications before potential exposure to HIV. This preventive strategy is recommended for individuals at high risk of HIV infection, such as those with HIV-positive partners.
4. Importance of Education:
4.1 Comprehensive Sexual Health Education: Education plays a pivotal role in STI prevention. Comprehensive sexual health education should cover topics such as safe sex practices, the importance of regular testing, and destigmatization of seeking medical care for STIs.
4.2 Promoting Communication and Consent: Education should emphasize the importance of open communication about sexual health with partners. Discussions about testing, STI status, and mutual consent contribute to responsible sexual practices.
5. Challenges in STI Prevention:
5.1 Stigma and Misinformation: Stigma surrounding STIs remains a significant barrier to prevention efforts. Misinformation, fear of judgment, and lack of awareness can hinder individuals from seeking testing, treatment, or adopting preventive measures.
5.2 Access to Healthcare: Limited access to healthcare services, especially in resource-limited settings, poses challenges to STI prevention. Barriers include economic constraints, inadequate healthcare infrastructure, and societal factors.
6. Public Health Interventions:
6.1 Community Outreach and Testing: Public health interventions involve community outreach programs that provide education, testing, and support. Mobile testing units, community clinics, and awareness campaigns aim to reach diverse populations and encourage regular testing.
6.2 Partner Notification Programs: Partner notification programs involve notifying individuals of potential exposure to an STI to encourage testing and preventive measures. These programs contribute to breaking the chain of transmission within communities.
7. Global Response and Research:
7.1 International Collaboration: Global organizations, governments, and non-governmental entities collaborate to address STIs on a global scale. Initiatives such as the World Health Organization’s Global Health Sector Strategy on STIs aim to guide countries in developing comprehensive responses.
7.2 Research and Innovation: Ongoing research focuses on developing new prevention methods, vaccines, and innovative strategies to address STIs. Continuous exploration of emerging challenges and evolving pathogens is critical for adapting prevention efforts.
8. Conclusion:
Understanding the dynamics of STI transmission and prevention is crucial for fostering responsible sexual health practices and mitigating the impact of these infections. Education, accessible healthcare, and global collaboration are key components of a comprehensive approach to STI prevention.
By promoting awareness, reducing stigma, and advocating for preventive measures, individuals and communities can contribute to breaking the cycle of transmission and fostering a healthier, more informed society.